Alzheimer’s disease is a progressive neurodegenerative disorder that primarily affects memory, thinking, and behavior. As the most common cause of dementia, it impacts millions of people worldwide. While aging is a well-known risk factor for Alzheimer’s, genetics also play a significant role in determining who is at risk of developing the disease. This blog will explore the complex relationship between genetics and Alzheimer’s, including the types of genetic influences, key genes involved, and the implications for diagnosis, treatment, and prevention.
Understanding Alzheimer’s Disease
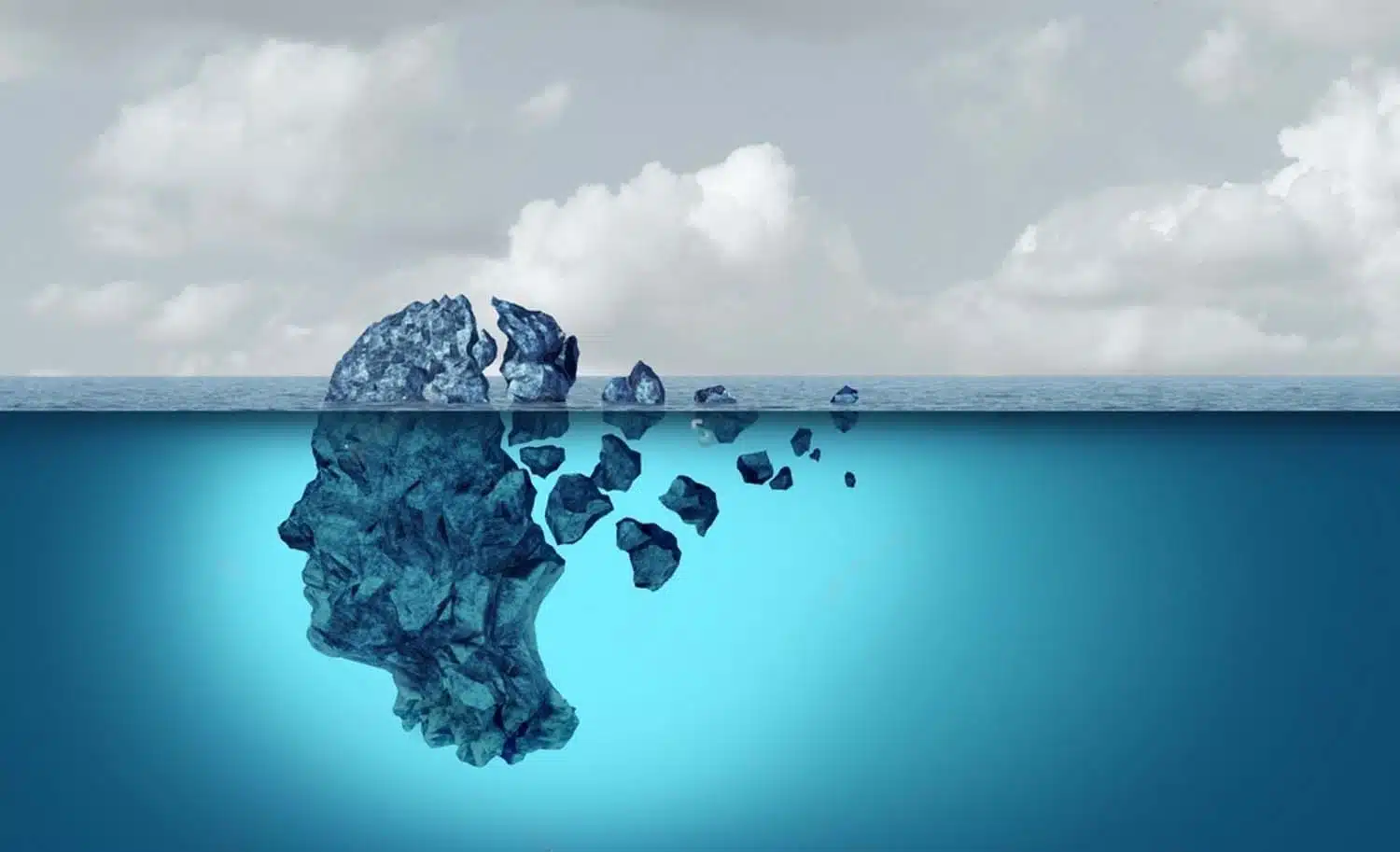
Before delving into the genetic aspects, it’s essential to understand the basic pathology of Alzheimer’s disease. Alzheimer’s is characterized by the accumulation of amyloid plaques and neurofibrillary tangles in the brain, leading to the death of neurons and loss of brain function. The disease progresses through several stages, from mild memory loss to severe cognitive impairment, ultimately leading to a complete dependency on others for care.
Genetic Influences on Alzheimer’s Disease
Genetic factors contribute to Alzheimer’s in two primary ways: through rare genetic mutations that directly cause the disease and through common genetic variations that influence the risk of developing it.
1. Early-onset Alzheimer’s Disease (EOAD)
Early-onset Alzheimer’s disease occurs in individuals younger than 65 and is relatively rare, accounting for less than 5% of all Alzheimer’s cases. EOAD often has a strong genetic component and is usually inherited in an autosomal dominant manner, meaning that inheriting one copy of the mutated gene from either parent can cause the disease. The three key genes associated with EOAD are:
- Amyloid Precursor Protein (APP) Gene: Mutations in the APP gene can lead to the overproduction of beta-amyloid, a protein fragment that forms the core of amyloid plaques in the brain. These plaques are a hallmark of Alzheimer’s disease.
- Presenilin 1 (PSEN1) Gene: Mutations in the PSEN1 gene are the most common cause of EOAD. PSEN1 mutations affect the production of a protein involved in the formation of amyloid plaques.
- Presenilin 2 (PSEN2) Gene: Like PSEN1, mutations in the PSEN2 gene also affect amyloid plaque formation, although they are less common.
Individuals with mutations in any of these genes almost invariably develop Alzheimer’s, often at a much younger age than those with the more common late-onset form.
2. Late-onset Alzheimer’s Disease (LOAD)
Late-onset Alzheimer’s disease typically manifests after the age of 65 and is the most common form of the disease. Unlike EOAD, LOAD is influenced by a combination of genetic, environmental, and lifestyle factors. Several genes have been identified that contribute to the risk of developing LOAD, with the most significant being the Apolipoprotein E (APOE) gene.
- APOE Gene: The APOE gene exists in three common variants (alleles): ε2, ε3, and ε4. The ε4 allele is the strongest genetic risk factor for LOAD. Individuals who inherit one copy of the ε4 allele have an increased risk, and those with two copies have an even higher risk. However, not everyone with the ε4 allele develops Alzheimer’s, and some people without it do, indicating that other genetic and environmental factors also play a role.
- In addition to APOE, genome-wide association studies (GWAS) have identified other genes associated with Alzheimer’s risk, including:
- Clusterin (CLU): Involved in the clearance of amyloid-beta from the brain.
- Phosphatidylinositol Binding Clathrin Assembly Protein (PICALM): Plays a role in synaptic function and endocytosis, processes essential for neuronal communication.
- Complement Receptor 1 (CR1): Involved in the immune response and amyloid-beta clearance.
These genes contribute to Alzheimer’s risk by influencing various biological pathways, such as amyloid-beta production and clearance, inflammation, lipid metabolism, and synaptic function.
Implications for Diagnosis and Treatment
Understanding the genetic underpinnings of Alzheimer’s disease has significant implications for diagnosis, treatment, and prevention.
1. Genetic Testing and Counseling
Genetic testing can identify individuals at risk of developing Alzheimer’s, particularly in families with a history of EOAD. Testing for mutations in the APP, PSEN1, and PSEN2 genes can provide valuable information for affected families. For LOAD, testing for the APOE ε4 allele can indicate an increased risk, although it cannot predict with certainty who will develop the disease.
Genetic counseling is crucial for individuals considering genetic testing. Counselors can help interpret test results, discuss the implications for family members, and provide support in making informed decisions about managing risk.
2. Targeted Therapies
Research into the genetic causes of Alzheimer’s is paving the way for the development of targeted therapies. For example:
a. Anti-Amyloid Therapies: Drugs aimed at reducing amyloid-beta production or enhancing its clearance are being developed, such as monoclonal antibodies that target amyloid plaques.
b. Gene Therapy: Emerging technologies like CRISPR could potentially be used to correct genetic mutations associated with EOAD, offering hope for future treatments.
3. Personalized Medicine
The growing understanding of the genetic factors involved in Alzheimer’s supports the move toward personalized medicine. By considering an individual’s genetic profile, healthcare providers can tailor prevention and treatment strategies to better address their specific risk factors.
Prevention and Risk Reduction
While genetic factors play a significant role in Alzheimer’s, they are not the sole determinants of the disease. Lifestyle and environmental factors also contribute, offering opportunities for risk reduction. Strategies to reduce Alzheimer’s risk include:
a. Healthy Diet: Diets rich in fruits, vegetables, whole grains, and lean proteins, such as the Mediterranean diet, are associated with a lower risk of Alzheimer’s.
b. Physical Activity: Regular exercise can improve cardiovascular health, which is linked to a reduced risk of cognitive decline.
c. Mental and Social Engagement: Staying mentally active and socially connected can help build cognitive reserve and delay the onset of symptoms.
d. Managing Cardiovascular Risk Factors: Controlling blood pressure, cholesterol, and diabetes can reduce the risk of Alzheimer’s and other forms of dementia.
The role of genetics in Alzheimer’s disease is complex and multifaceted. While certain genetic mutations can directly cause the disease, other genetic variations influence the risk. Understanding these genetic factors is crucial for early diagnosis, developing targeted therapies, and implementing personalized prevention strategies. At Shinon Healthcare, we are committed to providing comprehensive support and care for individuals and families affected by Alzheimer’s. Through advanced genetic testing, counseling, and innovative treatments, we aim to improve outcomes and enhance the quality of life for those at risk of or living with Alzheimer’s disease.